April 2008
Nutrition & Metabolism 2008
Abstract
Current nutritional approaches to metabolism syndrome and type 2 diabetes generally rely on reductions in dietary fat. The success of such approaches has been limited and therapy more generally relies on pharmacology. The argument is made that a re-evaluation of the role of carbohydrate restriction, the historical and intuitive approach to the problem, may provide an alternative and possibly superior dietary strategy. The rationale is based on the accepted idea that carbohydrate restriction improves glycemic control and reduces insulin fluctuations which are primary targets. Experiments are summarized showing that carbohydrate-restricted diets are at least as effective for weight loss as low-fat diets and that substitution of fat for carbohydrate is generally beneficial for risk of cardiovascular disease. These positive effects of carbohydrate restriction do not require weight loss. Finally, the point is re-iterated that carbohydrate restriction improves all of the features of metabolic syndrome.
Background
The epidemic of diabetes continues unabated, and impassioned calls for better treatment
and prevention strategies are common features of scientific conferences. While it is
generally acknowledged that total dietary carbohydrate is the major factor in glycemic
control, strategies based on reduction of dietary carbohydrate have received little support.
The American Diabetes Association, for example, has traditionally recommend against
low carbohydrate diets (less than 130 g/day[1]; while the most recent guidelines [2] admit
such diets as an alternative approach to weight loss, they continue to emphasize concerns
and downplay benefits. Similarly, Diabetes and Nutrition Study Group of the European
Association for the Study of Diabetes [3] reported “no justification for the
recommendation of very low carbohydrate diets in persons with diabetes.” We feel,
however, that there is ample evidence to warrant an alternative perspective and that diets
based on carbohydrate restriction should be re-evaluated in light of current understanding
of the underlying biochemistry and available clinical data.
Whatever success low fat dietary approaches have had in improving diabetes is to be
applauded but it is reasonable for patients to be aware of the potential benefits of an
alternative approach which we present here. The key feature is that low carbohydrate
diets are based on mechanism. That is, glucose directly or indirectly through insulin, is a
major control element in gluconeogenesis, glycogen metabolism, lipolysis and
lipogenesis. The downstream stimulus-response processes are a current research interest
(see e.g. [4, 5]) but, according to the view considered here, dietary fat has a generally
passive role and deleterious effects of fat are almost always seen in the presence of high
carbohydrate.
While low carbohydrate diets may not be appropriate for everyone, choices should be left
to individual physicians and patients. Key points that bear on the assessment of benefit
vs. risk of carbohydrate restriction are presented below. The discussion focuses on type 2
diabetes but many of the principles will apply to metabolic syndrome and possibly to type
1 as well[6, 7].
1. Carbohydrate restriction improves glycemic control, the primary target of
nutritional therapy and reduces insulin fluctuations.
2. Carbohydrate-restricted diets are at least as effective for weight loss as low-fat
diets.
3. Substitution of fat for carbohydrate is generally beneficial for markers for and
incidence of CVD.
4. Carbohydrate restriction improves the features of metabolic syndrome.
5. Beneficial effects of carbohydrate restriction do not require weight loss.
Carbohydrate restriction is an intuitive and rational approach to improvement of glycemic
and metabolic control. Data demonstrating that weight loss and cardiovascular risk are
also improved remove these barriers to the acceptance of carbohydrate restriction as a
reasonable if not the preferred treatment for type 2 diabetes. Finally, carbohydrate
restriction is a potentially favorable diet for improving components of the metabolic
syndrome and thereby for the prevention of diabetes.
1. Carbohydrate restriction improves glycemic control, the primary target of
nutritional therapy and reduces insulin fluctuations.
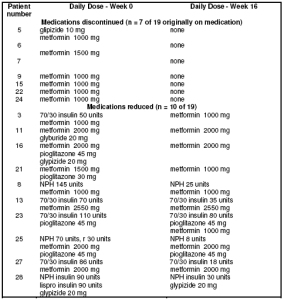
Figure 1 shows glycemic and insulin responses in a carefully controlled inpatient
comparison of 10 obese patients with type 2 diabetes[8]. Fourteen days of a lowcarbohydrate
diet led to a mean decrease in energy intake of approximately 1000 kcal/d, a
reduction in plasma glucose levels and average hemoglobin A1c (HbA1c) from 7.3% to
6.8%. Insulin sensitivity improved by approximately 75%. No adverse effects were
reported, and the carbohydrate that was removed was not replaced by substantial protein
or fat.
Dashti, et al. showed dramatic and sustained reduction in blood glucose in 31 obese
diabetic patients on a ketogenic diet over 56 weeks. Normal levels were reached by week
48 [9]. Similarly, Nielsen, et al.[10] reported that a 20 % carbohydrate diet was superior
to a 55-60 % carbohydrate diet with regard to bodyweight, glycemic control and
reduction in HbA1c.. At follow-up, after 22 months, HbA1c remained improved. In a 16-
week pilot study of Yancy, et al., 21 overweight participants with type 2 diabetes showed
a mean decrease in HbA1c from 7.4 % to 6.3 %.
These results are not isolated. Many studies have demonstrated the benefits of
carbohydrate reduction[11-16] on glycemic control. Reaven, Garg, Grundy and
coworkers have shown benefits of even moderate carbohydrate reduction, from 55% to
40%[17, 18].
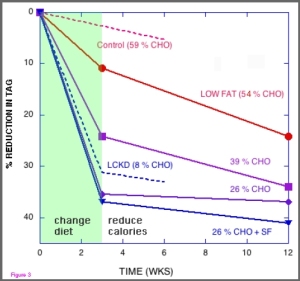
Reduction or elimination of medication.
A striking effect of carbohydrate restriction is reduction or elimination of medication.
Table 1 shows results from Yancy, et al. [19] in which 17 of 21 patients with type 2
diabetes reduced or discontinued diabetes medication upon carbohydrate restriction.
Similar results were found by Boden [8] and Nielsen [10, 20]. Practitioners have pointed
out the need to reduce medication in advance of undertaking a low carbohydrate diet [6,
10, 20, 21] highlighting the power of carbohydrate restriction to bring about the same
therapeutic effect as drugs.
2. Carbohydrate-restricted diets are at least as effective for weight loss as low-fat
diets.
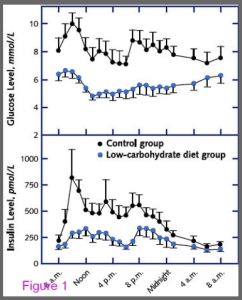
Low-carbohydrate diets generally perform better than low-fat diets for weight loss in
normal subjects, and patients with metabolic syndrome or diabetes[22-25]. Studies by
Foster, et al. [26] and Samaha, et al. [27] are often cited as examples where low
carbohydrate diets are more effective at 6 months but no better than low-fat diets at 1
year. The experimental design, however, allowed re-introduction of carbohydrate in the
low carbohydrate group as the study proceeded. Even if there were equal weight loss at
one year, other physiologic markers, particularly TG and HDL, were greatly improved on
the low-carbohydrate diet compared with the high carbohydrate diet as shown in Figure 2.
3. Substitution of fat for carbohydrate is generally beneficial for markers for and
incidence of CVD.
The diet-heart hypothesis states that dietary fat, or at least saturated fat, promotes CVD.
There are, however, numerous counter-examples and the popular and scientific literature
has seriously challenged many of the underlying assumptions of the hypothesis [28-33].
In fact, total fat in the diet is not associated with an increase in CVD, as shown by
experiments going back to Ancel Keys’s Seven Country Study [34]and, most recently
and dramatically, the Women’s Health Initiative [35].
Lipid markers for CVD
Clinically significant elevation of LDL-cholesterol is generally considered a primary
indicator of CVD risk but interpretation must be tempered by the effect of particle size:
small dense LDL particles are significantly more atherogenic than large, buoyant LDL
particles [36, 37]. Krauss, et al. identified a genetically influenced pattern (B) in people
with higher levels of the smaller particles and found a strong linear relation between
carbohydrate intake and prevalence of the atherogenic pattern B phenotype. Thus,
replacing dietary fat with carbohydrate tends to worsen LDL size distribution for most of
the population[36, 37].
Other factors, such as high triglyceride (TG) and low HDL, are independent markers of
insulin resistance and CVD risk. Indeed, the triglyceride:HDL ratio has been posited to
be a surrogate measure of insulin resistance [38]. This ratio is frequently exacerbated
under conditions that lower LDL [24]. An increase in apolipoprotein B (apoB) may be a
preferred marker since each atherogenic lipoprotein particle contains one molecule of
apoB; total LDL would bias results towards lower risk [39]. There is also strong
evidence that the apoB/apoA-I ratio is superior to conventional cholesterol ratios [39] as
a predictor of CVD risk. Of particular importance is circulating TG because of its
mechanistic link to the formation of atherogenic particles [40, 41], and its responsiveness
to dietary manipulation. There is probably no dietary outcome as reliable as the reduction
in TG due to carbohydrate restriction[41].
The role of saturated fat.
A primary goal of current recommendations is to put limits on dietary saturated fat but
published results are inconsistent (see e.g. [42]). Several critical reviews have pointed up
the general failure to meet the kind of unambiguous outcomes that would justify blanket
condemnation of saturated fat, per se.[29, 30, 41, 43, 44]. Notably, during the obesity
and diabetes epidemic, the proportion of dietary saturated fat decreased. In men, the
absolute amount decreased by 14 %. Similarly, the WHI revealed no difference in CVD
incidence for people who consumed < 10 % saturated fat or those whose consumption
was > 14 %[35]. Dreon, et al.[44] showed that increased saturated fat lead to a decrease
in small, dense LDL. Perhaps most remarkable was a study by Mozaffarian [45] which
showed that greater intake of saturated fat was associated with reduced progression of
coronary atherosclerosis; greater carbohydrate intake was linked to increased progression.
In our view, inconsistencies in the experimental results with dietary saturated fat arise
from a failure to distinguish between replacement by unsaturated fat or by carbohydrate
[3]. In the former case, there is usually improvement in CVD risk or outcome (although
it is not excluded that this is due to the effect of the unsaturated fat rather than reduction
in the risk from the saturated fat). Replacement of saturated fat with carbohydrate,
however, is almost always deleterious [46, 47]. Again, the idea that carbohydrate is a
control element determining the fate of ingested lipid is overriding.
The assumption that the dietary fatty acid profile is reflected in plasma distribution is not
always true, especially for saturated fatty acids which seems to be subject to much
metabolic processing [42]. It was also expected that an increase in total fat might show
changes in lipid pattern but Raatz, et al. showed that such differences were extremely
small between a low fat and high fat diet [48]. A recent report comparing two low-CHO
groups that differed in dietary SFA showed little difference in plasma levels of stearic or
palmitic acid [49]. Most telling, Volek’s group compared a VLCK diet (% CHO:fat
12:59) with a low-fat (LF) diet (56:24) and found that after 12 weeks, SFA in TG and
cholesteryl ester were lower in the VLCK group than the LF group even thought the low
carbohydrate group had a 3-fold higher intake of dietary SFA [50].
4. Carbohydrate restriction improves the features of metabolic syndrome.
An important idea guiding current medical thinking is that clustering of seemingly
disparate physiologic states, obesity, atherogenic dyslipidemia, hyperglycemia and
hypertension, termed metabolic syndrome (MetS) suggests a common underlying cause.
Inherent in this concept lies the possibility that treating one risk factor or disease state
might confer benefit for risk of other diseases. A recent review showed that carbohydrate
restriction improves all of these markers[24]. Indeed, metabolic syndrome might be
consistently defined as those physiologic markers that respond to reduction in dietary
carbohydrate. Metabolic syndrome might be seen as a generalization of the carbohydrate
intolerance that characterizes frank diabetes[24].
In a prospective study testing the hypothesis linking carbohydrate restriction to MetS, the
carbohydrate-restricted group showed greater improvements in weight loss and multiple
markers of atherogenic dyslipidemia (increased HDL and LDL diameter and reductions
in TG and apo B/apo A1 ratio) compared to a low fat arm. Unexpectedly, the
carbohydrate-restricted arm, with three times greater dietary saturated fat, showed a
reduction in plasma saturated fat, while plasma saturated fat in the low-fat arm remained
unchanged [50].
Similarly, Petersen, et al. [51] showed that ingestion of a high carbohydrate meal led to a
greater increase in de novo fatty acid synthesis and hepatic triglyceride formation in
insulin-resistant men compared to a similar group of insulin-sensitive controls.
Carbohydrate-induced atherogenic dyslipidemia is thus enhanced by insulin resistance.
Carbohydrate restriction will generally reduce the consumption of fructose, which makes
up half the mass of common sweeteners (high-fructose corn syrup or sucrose). Fructose
consumption has been implicated in the epidemics of obesity, MetS, and type 2 diabetes
and is known to induce hypertension, de novo lipogenesis, hepatic insulin resistance and
adiposity[52-54].
In summary, carbohydrate restriction is one of the few common interventions that targets
all of the features of MetS. If such a straight-forward approach can alleviate a condition
for which there is no known effective drug, its potential should be vigorously explored.
5. Beneficial effects of carbohydrate restriction do not require weight loss.
Obesity is commonly considered a cause of insulin resistance. Obesity, however, does not
occur spontaneously. Obesity is a response. The effects of obesity that lead to insulin
resistance in peripheral tissues, largely increased fatty acids, are downstream from the
primary impact of diet. This argues for an emphasis of treatment on glycemic control
and improved hepatic metabolism rather than weight loss. A simpler alternative
hypothesis considers that insulin resistance represents a down-regulation of hormonal
response as a result of persistent high levels of insulin, a feature common to other
hormonal systems [55]. In this view, diabetes, obesity and the components of MetS are
parallel effects of hyperinsulinemia and/or hyperglycemia.
The finding that lipid improvements seen in carbohydrate-restricted diets persist even
after no further weight loss (Figure 2) suggests that the benefit of carbohydrate
restriction is independent of weight loss. Two additional lines of evidence support this
idea:
1) In experiments in which body mass is kept constant in normal-weight men[56]or
patients with type 2 diabetes[11, 13], a very low carbohydrate diet resulted in dramatic
improvements in triglycerides and HDL cholesterol with minimal change in body mass.
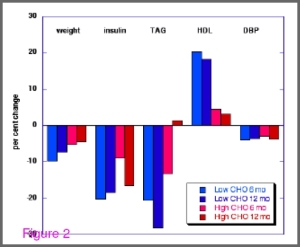
2) Experiments in which change in macronutrients and weight loss are separated in time
show that eucaloric carbohydrate reduction leads to greater improvement in atherogenic
lipid markers (TG, HDL, apoB/apoA-1 and mean LDL particle size) even in the presence
of higher saturated fat[57, 58]. A low fat diet, however, required weight loss to achieve
effective improvement in the lipid profile (Figure 3). Notably, the sum of the two effects
showed that eucaloric carbohydrate restriction plus weight loss was more effective than
eucaloric low fat plus weight loss.
Practical considerations and recommendations.
Definitions and recommendations
Response to carbohydrate restriction shows both continuous, graded outcomes [17, 18] as
well as a threshold effects. LDL particle size, e.g. appears to depend linearly on the level
of dietary carbohydrate[36, 37]. On the other hand, many studies show maximum benefit
for very low carbohydrate intake; the early phases of popular low carbohydrate diets
target such very low levels [6, 15, 21, 59, 60]. The principle rests on the concept of a
catalytic or threshold effect for insulin in shifting the body from an anabolic state to fat
oxidation. The tipping point is empirically taken as the onset of ketonuria, also used as an
indicator of compliance with a very low carbohydrate ketogenic diet (VLCKD). The
threshold carbohydrate reduction for ketonuria varies among individuals, but a rough
estimate is 50 g of carbohydrate per day or, approximately 10 % of energy on a nominal
2000 kcal diet, (a target of 30 g/d is common in the early phases of popular VLCKD
diets)[15, 21, 60].
We suggest the following definitions:
The ADA designates low carbohydrate diets as less than 130 g/d or 26% of a nominal
2000 kcal diet and we consider this a reasonable cutoff for the definition of a low-
carbohydrate diet. Carbohydrate consumption before the epidemic of obesity averaged
43%, and we suggest 26% to 45% as the range for moderate-carbohydrate diets. The
intake of less than 30 g/d, as noted above should be referred to as a very low
carbohydrate ketogenic diet (VLCKD). The term Ketogenic Diet should be reserved for
the therapeutic approach to epilepsy. These diets do not independently specify the level
of carbohydrate, but rather the sum of carbohydrate and protein.
In practice, many low carbohydrate dieters do not add additional fat. First shown by
LaRosa, [61] it has now been observed by many other investigators. [8, 62, 63] A
reduced carbohydrate diet may show significant per cent increase in fat, but there may be
no change in the absolute amount consumed. Not everybody on a low carbohydrate diet
follows this pattern, but a recommendation based on this behavior would seem more
appropriate than unqualified rejection of low-carbohydrate diets.
While some proponents of carbohydrate restriction for the management of diabetes favor
sustained adherence to very low levels of carbohydrate intake [6], all options may be
considered and therapeutic choices can be determined by individual physicians and their
patients
The term low-carbohydrate diet is frequently taken as synonymous with the popular
Atkins diet[60] which remains highly controversial. Carbohydrate control, however, has
many implementations and the severity of the epidemic of diabetes makes it appropriate
to go beyond historical controversy and analyze dietary interventions as they are actually
implemented.
There is reluctance to make recommendations for low carbohydrate diets on the grounds
that people will not follow them but compliance and efficacy of dietary recommendations
are separate phenomena. In fact, all recommendations are specifically intended to be
different from average consumption[1] and it is sensibly the purpose of health agencies to
encourage conformance to the best therapies.
It is time to re-appraise the role of carbohydrate restriction. Although pessimism exists in
the medical community on the efficacy of any diet in the treatment of diabetes 2 and
MetS, the success of carbohydrate restriction for many practitioners and individual
patients[64] mandates that we should determine how this approach can be consistently
and effectively employed.
Finally, while no systematic study of clinical practice has been done, anecdotal evidence
suggests that carbohydrate restriction is a common clinical recommendation for diabetes.
We believe that there is a need to codify these recommendations in light of current
evidence.
Basic biochemistry, clinical experience and an evolving understanding of metabolic
syndrome support the need for evaluation of the efficacy and safety of carbohydraterestricted
diets for the treatment of type 2 diabetes. The fact that carbohydrate restriction
improves markers of cardiovascular health, even in the absence of weight loss, sensibly
removes historical objections to the dangers of this approach. A critical re-appraisal
could form the basis for an alternative for those patients for whom current
recommendations are not successful.
Competing interests
MCV has been a consultant for Atkins Nutritionals, Inc. All other authors declare that
they have nothing to declare.
Authors’ contributions
RDF wrote the first version of this article based on published material and
correspondence with the other authors who modified and approved the final version.
References
1. American Diabetes Association: Nutrition Recommendations and
Interventions for Diabetes–2007. Diabetes Care 2007, 30(Suppl 1):S48-S65.
2. American Diabetes Association: Nutrition Recommendations and
Interventions for Diabetes–2008. Diabetes Care 2008, 31(Suppl 1):S61-S78.
3. Mann JI, De Leeuw I, Hermansen K, Karamanos B, Karlstrom B, Katsilambros
N, Riccardi G, Rivellese AA, Rizkalla S, Slama G et al: Evidence-based
nutritional approaches to the treatment and prevention of diabetes mellitus.
Nutr Metab Cardiovasc Dis 2004, 14(6):373-394.
4. Draznin B: Molecular mechanisms of insulin resistance: serine
phosphorylation of insulin receptor substrate-1 and increased expression of
p85alpha: the two sides of a coin. Diabetes 2006, 55(8):2392-2397.
5. Reusch JE, Draznin BB: Atherosclerosis in diabetes and insulin resistance.
Diabetes Obes Metab 2007, 9(4):455-463.
6. Bernstein R: Dr. Bernstein’s Diabetes Solution: The Complete Guide to Achieving
Normal Blood Sugars: Little, Brown and Company; 2007.
7. Nielsen JV, Jonsson E, Ivarsson A: A low carbohydrate diet in type 1 diabetes:
clinical experience–a brief report. Ups J Med Sci 2005, 110(3):267-273.
8. Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP: Effect of a lowcarbohydrate
diet on appetite, blood glucose levels, and insulin resistance in
obese patients with type 2 diabetes. Ann Intern Med 2005, 142(6):403-411.
9. Dashti HM, Mathew TC, Khadada M, Al-Mousawi M, Talib H, Asfar SK,
Behbahani AI, Al-Zaid NS: Beneficial effects of ketogenic diet in obese
diabetic subjects. Mol Cell Biochem 2007.
10. Nielsen JV, Joensson EA: Low-carbohydrate diet in type 2 diabetes. Stable
improvement of bodyweight and glycaemic control during 22 months followup.
Nutr Metab (Lond) 2006, 3(1):22.
11. Allick G, Bisschop PH, Ackermans MT, Endert E, Meijer AJ, Kuipers F,
Sauerwein HP, Romijn JA: A low-carbohydrate/high-fat diet improves
glucoregulation in type 2 diabetes mellitus by reducing postabsorptive
glycogenolysis. J Clin Endocrinol Metab 2004, 89(12):6193-6197.
12. Daly ME, Paisey R, Paisey R, Millward BA, Eccles C, Williams K, Hammersley
S, MacLeod KM, Gale TJ: Short-term effects of severe dietary carbohydraterestriction
advice in Type 2 diabetes–a randomized controlled trial. Diabet
Med 2006, 23(1):15-20.
13. Gannon MC, Nuttall FQ: Control of blood glucose in type 2 diabetes without
weight loss by modification of diet composition. Nutr Metab (Lond) 2006, 3:16.
14. Vernon M, Mavropoulos J, Transue M, Yancy W, Jr, Westman E: Clinical
Experience of a Carbohydrate-Restricted Diet: Effect on Diabetes Mellitus.
Metabolic Syndrome and Related Disorders 2003, 1:233-237.
15. Vernon MC, Eberstein JA: Atkins Diabetes Revolution. The Groundbreaking
Approach to Preventing and Controlling Type 2 Diabetes. New York: William
Morrow; 2004.
16. Yancy WS, Jr., Vernon MC, Westman EC: A Pilot trial of a Low-
Carbohydrate, Ketogenic Diet in Patients with Type 2 Diabetes. Metabolic
Syndrome and Related Disorders 2003, 1(3):239-243.
17. Reaven GM: Effect of dietary carbohydrate on the metabolism of patients
with non-insulin dependent diabetes mellitus. Nutr Rev 1986, 44(2):65-73.
18. Garg A, Bantle JP, Henry RR, Coulston AM, Griver KA, Raatz SK, Brinkley L,
Chen YD, Grundy SM, Huet BA et al: Effects of varying carbohydrate content
of diet in patients with non-insulin-dependent diabetes mellitus. JAMA 1994,
271(18):1421-1428.
19. Westman EC, Yancy Jr. WS, Haub MD, Volek JS: Insulin Resistance from a
Low-Carbohydrate, High Fat Diet Perspective. Metabolic Syndrome and
Related Disorders 2005, 3:3-7.
20. Nielsen JV, Jonsson E, Nilsson AK: Lasting improvement of hyperglycaemia
and bodyweight: low-carbohydrate diet in type 2 diabetes–a brief report.
Ups J Med Sci 2005, 110(1):69-73.
21. Eades MR, Eades MD: Protein Power. New York: Bantam Books; 1996.
22. Feinman RD, Fine EJ: Thermodynamics and Metabolic Advantage of Weight
Loss Diets. Metabolic Syndrome and Related Disorders 2003, 1:209-219.
23. Krieger JW, Sitren HS, Daniels MJ, Langkamp-Henken B: Effects of variation
in protein and carbohydrate intake on body mass and composition during
energy restriction: a meta-regression 1. Am J Clin Nutr 2006, 83(2):260-274.
24. Volek JS, Feinman RD: Carbohydrate restriction improves the features of
Metabolic Syndrome. Metabolic Syndrome may be defined by the response
to carbohydrate restriction. Nutr Metab (Lond) 2005, 2:31.
25. Westman EC, Feinman RD, Mavropoulos JC, Vernon MC, Volek JS, Wortman
JA, Yancy WS, Phinney SD: Low-carbohydrate nutrition and metabolism. Am
J Clin Nutr 2007, 86(2):276-284.
26. Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary
PO, Rader DJ, Edman JS, Klein S: A randomized trial of a low-carbohydrate
diet for obesity. N Engl J Med 2003, 348(21):2082-2090.
27. Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams T,
Williams M, Gracely EJ, Stern L: A low-carbohydrate as compared with a lowfat
diet in severe obesity. N Engl J Med 2003, 348(21):2074-2081.
28. Colpo A: The Great Cholesterol Con: Lulu Press; 2006.
29. German JB, Dillard CJ: Saturated fats: what dietary intake? Am J Clin Nutr
2004, 80(3):550-559.
30. Karam J, Nessim F, McFarlane S, Feinman R: Carbohydrate Restriction and
Cardiovascular Risk. Current Cardiovascular Risk Reports 2008, 2(2):88-94.
31. Ravnskov U: The Cholesterol Myths: Exposing the Fallacy that Cholesterol and
Saturated Fat Cause Heart Disease. Washington, DC: NewTrends Publishing,
Inc.; 2000.
32. Taubes G: Good Calories, Bad Calories. New York: Alfred A. Knopf; 2007.
33. Volek JS, Forsythe CE: The case for not restricting saturated fat on a low
carbohydrate diet. Nutr Metab (Lond) 2005, 2:21.
34. Keys A: Coronary heart disease in seven countries. 1970, 41 (Suppl):1-211.
35. Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller
S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL et al: Low-fat dietary pattern
and risk of cardiovascular disease: the Women’s Health Initiative
Randomized Controlled Dietary Modification Trial. JAMA 2006, 295(6):655-
666.
36. Dreon DM, Fernstrom HA, Miller B, Krauss RM: Low-density lipoprotein
subclass patterns and lipoprotein response to a reduced-fat diet in men.
FASEB J 1994, 8(1):121-126.
37. Krauss RM: Atherogenic lipoprotein phenotype and diet-gene interactions. J
Nutr 2001, 131(2):340S-343S.
38. McLaughlin T, Reaven G, Abbasi F, Lamendola C, Saad M, Waters D, Simon J,
Krauss RM: Is there a simple way to identify insulin-resistant individuals at
increased risk of cardiovascular disease? Am J Cardiol 2005, 96(3):399-404.
39. Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture
P, de Graaf J, Durrington PN, Faergeman O, Frohlich J et al: Apo B versus
cholesterol in estimating cardiovascular risk and in guiding therapy: report
of the thirty-person/ten-country panel. J Intern Med 2006, 259(3):247-258.
40. Ginsberg HN, Zhang YL, Hernandez-Ono A: Regulation of plasma
triglycerides in insulin resistance and diabetes. Arch Med Res 2005, 36(3):232-
240.
41. Volek JS, Sharman MJ, Forsythe CE: Modification of lipoproteins by very lowcarbohydrate
diets. J Nutr 2005, 135(6):1339-1342.
42. Vessby B: Dietary fat, fatty acid composition in plasma and the metabolic
syndrome. Curr Opin Lipidol 2003, 14(1):15-19.
43. Ravnskov U: The questionable role of saturated and polyunsaturated fatty
acids in cardiovascular disease. J Clin Epidemiol 1998, 51(6):443-460.
44. Dreon DM, Fernstrom HA, Campos H, Blanche P, Williams PT, Krauss RM:
Change in dietary saturated fat intake is correlated with change in mass of
large low-density-lipoprotein particles in men. Am J Clin Nutr 1998,
67(5):828-836.
45. Mozaffarian D, Rimm EB, Herrington DM: Dietary fats, carbohydrate, and
progression of coronary atherosclerosis in postmenopausal women. Am J Clin
Nutr 2004, 80(5):1175-1184.
46. Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens
CH, Willett WC: Dietary fat intake and the risk of coronary heart disease in
women. N Engl J Med 1997, 337(21):1491-1499.
47. Mensink RP, Zock PL, Kester AD, Katan MB: Effects of dietary fatty acids and
carbohydrates on the ratio of serum total to HDL cholesterol and on serum
lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin
Nutr 2003, 77(5):1146-1155.
48. Raatz SK, Bibus D, Thomas W, Kris-Etherton P: Total fat intake modifies
plasma fatty acid composition in humans. J Nutr 2001, 131(2):231-234.
49. Cassady B, Charboneau N, Brys E, Crouse K, Beitz D, Wilson T: Effects of low
carbohydrate diets high in red meats or poultry, fish and shellfish on plasma
lipids and weight loss. Nutr Metab (Lond) 2007, 4(23).
50. Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM,
Kraemer WJ, Feinman RD, Volek JS: Comparison of low fat and low
carbohydrate diets on circulating Fatty Acid composition and markers of
inflammation. Lipids 2008, 43(1):65-77.
51. Petersen KF, Dufour S, Savage DB, Bilz S, Solomon G, Yonemitsu S, Cline GW,
Befroy D, Zemany L, Kahn BB et al: Inaugural Article: The role of skeletal
muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc
Natl Acad Sci U S A 2007, 104(31):12587-12594.
52. Le KA, Tappy L: Metabolic effects of fructose. Curr Opin Nutr Metab Care
2006, 9:469-475.
53. Rutledge AC, Adeli K: Fructose and the metabolic syndrome:
pathophysiology and molecular mechanisms. Nutr Rev 2007, 65(6):S13-S23.
54. Zammit VA: Insulin stimulation of hepatic triacylglycerol secretion in the
insulin-replete state: implications for the etiology of peripheral insulin
resistance. Ann N Y Acad Sci 2002, 967:52-65.
55. Lustig RH: Childhood obesity: behavioral aberration or biochemical drive?
Reinterpreting the First Law of Thermodynamics. Nature Clin Pract Endo
Metab 2006, 2:447-458.
56. Sharman MJ, Kraemer WJ, Love DM, Avery NG, Gomez AL, Scheett TP, Volek
JS: A ketogenic diet favorably affects serum biomarkers for cardiovascular
disease in normal-weight men. J Nutr 2002, 132(7):1879-1885.
57. Feinman RD, Volek JS: Low carbohydrate diets improve atherogenic
dyslipidemia even in the absence of weight loss. Nutr Metab (Lond) 2006, 3:24.
58. Krauss RM, Blanche PJ, Rawlings RS, Fernstrom HS, Williams PT: Separate
effects of reduced carbohydrate intake and weight loss on atherogenic
dyslipidemia. Am J Clin Nutr 2006, 83(5):1025-1031.
59. Agatston A: The South Beach Diet. New York: Random House; 2003.
60. Atkins RC: Dr. Atkins’ New Diet Revolution. New York: Avon Books; 2002.
61. Larosa JC, Fry AG, Muesing R, Rosing DR: Effects of high-protein, lowcarbohydrate
dieting on plasma lipoproteins and body weight. J Am Diet
Assoc 1980, 77(3):264-270.
62. Yancy WS, Jr., Foy M, Chalecki AM, Vernon MC, Westman EC: A lowcarbohydrate,
ketogenic diet to treat type 2 diabetes. Nutr Metab (Lond) 2005,
2:34.
63. Volek JS, Sharman MJ, Gomez AL, Judelson DA, Rubin MR, Watson G, Sokmen
B, Silvestre R, French DN, Kraemer WJ: Comparison of energy-restricted very
low-carbohydrate and low-fat diets on weight loss and body composition in
overweight men and women. Nutr Metab (Lond) 2004, 1(1):13.
64. Feinman RD, Vernon MC, Westman EC: Low carbohydrate diets in family
practice: what can we learn from an internet-based support group. Nutr J
2006, 5:26.
Figures
Figure 1 – Glucose and Insulin response for patients with type 2 diabetes on low
carbohydrate diet vs. control.
Data (means ± SE ) are for 9 patients with type 2 diabetes after seven days on their usual
high-carbohydrate diet (control) and after 2 weeks) on a low-carbohydrate diet.
Medication was reduced in 4 patients and discontinued in one during the lowcarbohydrate
diet. Figure redrawn from Boden, et al. [8].
Figure 2 – Comparison of low and high carbohydrate diets at 6 and 12 months.
Results from a multi-center trial in which 63 obese men and women were randomly
assigned to either diet. Data from Foster, et al. [26]. Figure from Volek & Feinman [24],
used with permission.
Figure 3 – Effect of dietary interventions on reduction in TAG
Eucaloric diets of indicated carbohydrate content were begun at time 0. At week 3, a
1000 kcal reduction in energy was implemented and at week 9, dieters were put on
maintenance diet. Combined effect of calorie reduction and maintenance are reported at
week 12.
Solid Lines: data from Krauss, et al. [58] were converted from reported log values in
their Table 2 and per cent of baseline was calculated.
Dashed line: data from Sharman , et al [56]: A eucaloric ketogenic diet was instituted for
six weeks (no weight loss phase). Points were recorded at week 3 and 6. Figure
modified from Feinman & Volek [57]. Similar results were found for HDL, apoB/apoA1
and other markers of CVD [57, 58]
Table 1. Changes in diabetes medication of 19 overweight participants with type 2
diabetes who underwent a 16-week diet intervention trial. Patients were provided with
LCKD counseling with an initial goal of <20 g carbohydrate/day. Medication were
reduced at diet initiation. Data from Yancy, et al.[62].
Nutrition & Metabolism 2008, 5:9doi:10.1186/1743-7075-5-9